The Pressing Need For Needle-Free Immunization With Heather Callender-Potters

Immunization is an important subject to talk about, especially in the midst of a pandemic like COVID-19. While traditional immunization methods are popular as ever, more and more companies are seeking out methods for needle-free immunization that mitigate some of the risks presented by needle immunization. Bob Roark is joined by Heather Callender-Potters, the Co-Founder of PharmaJet, to discuss the pressing impetus for investing more resources into needle-free immunization. Let Bob and Heather take you through this vital topic with a spirited conversation.
—
Watch the episode here:
https://www.youtube.com/watch?v=zYQTMdkD5qI
The Pressing Need For Needle-Free Immunization With Heather Callender-Potters
My guest is Heather Potters. She’s the Vice Chairman, Global Business Development Officer, and Cofounder of PharmaJet. Welcome, Heather.
It’s exciting for me. Thank you.
I’m so excited to have this time with you and get your story out there, which it’s already out there, but at least through this channel. If you could talk about PharmaJet’s vision and your vision is needle-free applications for immunization and the story of why you started there and why that’s still your focus.
My mother and me cofounded the business. We wanted to make sure that we made a contribution to healthcare. She had experienced needles, she’d seen reused and there was a call to action by the World Health Organization because they were witnessing needle reuse about whether or not somebody could develop a needle-free immunization tool. We decided to rise to that occasion. When we looked at the market, immunization is global. We all share the healthcare burden. We’re in the midst of something around Coronavirus where it’s abundantly clear that if people are healthy, they’re at work, the economy works. If a group of people is healthy, then the population generally is healthy. We focused on what we could do around taking needles out of the garbage dumps and the risk of reuse and needlestick and then that immunization market that’s growing in perpetuity.
More people being born, more need for immunization. If you fast forward to where we are, the exciting thing is that over time we’ve been able to prove that you might be able to move from the muscle to the skin and functionally reduce the dose of the vaccine by 80% and get the same immune response. It’s nifty. It’s around the immunology that our skin has. Our body’s barriers are always protecting us from things. The other exciting thing is that we kept seeing this glimmer of making vaccines work better. In particular in nucleic acid vaccines, messenger RNA, and DNA vaccines, we tend to see a multiple of higher immune response versus needle-based delivery. There’s a whole slew of things, whether or not it’s infectious disease or oncology, things coming to market to address disease concerns that we don’t have treatment for. Like on the infectious disease side, it could be Zika and now also COVID. On the oncology side, it could be someone who’s manifested HPV, cervical cancer, lung cancer, or leukemia. Lots of things that give us joy around near-term immunization, medium-term, reduce the dose in the longer-term of bringing things to market that don’t have vaccine cures.

Needle-Free Immunization: A significant percentage of people avoid immunization because they don’t like needles.
Thinking about the mechanics, my memory goes back to when I was a little boy. I got my polio sugar cube with a little red dot on it. We have certainly progressed a long way since then. For you with the jet injection, what role do you think that’s going to play going forward in the immunization market?
Polio is a standing example because we have that short-term memory or frankly, the older you are, the more you remember about the polio risk. There were people who are basically going swimming feeling fine and the next day, not able to walk, not able to breathe. Things like iron lungs in the ‘50s. That’s a distant memory for most people. The oral drops on the sugar cube essentially were discontinued from use in places like the United States because they have a live virus. However, they’re inexpensive. The use of oral drops has been continued in the rest of the world. Thanks to the leadership of the Bill & Melinda Gates Foundation, CDC, there’s been a drive towards adopting those as the standard of care to bring the disease incidents down.
In fact, if you’re exposed to polio and you’re not immunized, you have 1 in 200 risks of getting polio and manifesting some form of paralysis that is irreversible. Given that the disease incidence has come down, it’s now time to eradicate the disease. The injectable inactivated vaccine that we use as a standard of care here and in numerous countries has been mostly used in the developing world. Now it’s time to adopt that safer vaccine that doesn’t have the live riders in order to get rid of the virus from the planet truly. While we’re close, by no means has polio been eradicated. The exciting thing for PharmaJet is that we’ve been part of this journey with the WHO leading the charge and the Bill & Melinda Gates Foundation and CDC around how to eradicate it, but afford eradication.
They were dropped to about $0.18. The injectable polio vaccine is about $3 in the cheapest of UNICEF pricing, twenty times more expensive. How do you bridge that gap? We are a tool where we’ve been able to prove that you can move from the muscle to the skin. Functionally 60% less vaccine injected into generally using our device is superior in the immune response to a full dose into the muscle. It took a long time to prove that and that’s a credential that the World Health Organization, a scientific advisory group of experts opined on, which we enjoy now. If you add further, we get functionally 20% more out of the vials versus needles because we’ve engineered out all of the waste and then push and click up against the body. Any caregiver can deliver that shot and then there are no needle shots to take away, which is also an extra cost. Lastly, we inspire more people to be immunized. We traditionally find a significant percentage of people avoid immunization because they don’t like needles and many of those people will participate. It’s around that herd immunity, more people immunized moving to the safer vaccine to truly, fully then eradicate polio from the planet.
In the immunization side, there’s the mechanical feature. Many don’t like shots. I don’t know of anybody that said, “I love to get them.” Also, aren’t there some cultural barriers in some countries against needle-based immunization?
There are. It’s an interesting topic because in the United States we want it to be safe, comfortable, and perfect. It’s whatever the services that we’re getting whether or not it’s healthcare or going off to McDonald’s. In certain parts of the rest of the world, there are people who don’t like to see blood, particularly in the Muslim world. Consequently, we have a leg up in terms of this noninvasive method of administration. We formed a fast, fluid injection so it goes into the body in less than a tenth of a second, faster than your nervous system can respond. That fluid is traveling quickly and it’s the size of two human hairs.
If we wanted to call it magic, that would be easier. We basically get rid of that needle experience and the angst that goes along with that as well. We can’t claim that it’s pain-free or that you might not see a drop of blood or fluid because we do a small hole, but it’s much less invasive, much more patient-friendly, and certainly caregiver friendly. While there are places that pride themselves on if it hurts, it worked, the chief is that most healthcare workers don’t want to hurt their patients. There’s a much more comfortable way to receive an immunization.
Circling back around to that, your mom, was she a dentist?
She became a dental hygienist and she worked with my father and ran his practices. My dad has three board certifications. He’s also retired and older, but they did volunteer medicine and dentistry together in various countries. That’s where she was struck by the fact that we all take for granted the healthcare that we have here. If you live in simple means, you make do with what you have. If you don’t have much, you’re probably going to reuse some of the things that you have. The whole concept of needlestick and risk of reuse was something that touched her.

Needle-Free Immunization: With needle-free vaccines, we could effectively immunize people while still maintaining a significantly positive patient experience.
I think about the evolution of that. I worked in a hospital early on when I was in college and there wasn’t much protocol about disposing of needles. They went where they went. The HIV world showed up and the side of the needle of the house became much more prevalent, apparent, or aware. This issue that we have now with the Coronavirus, I’m wondering if that’s not a tipping point. There’s been an anti-vaxxer movement that’s out around doing what they do. It’s a call to arms. I would seem to think that this will be an amazing call to arms for technology like yours.
I appreciate that and I want to make sure that people know that we’ll never get rid of these because they can be important and useful. We happen to be basically the only alternative for vaccine delivery for a needle-free jet injection technology. One, it’s around the credentials that we have. The FDA and CE mark. We’re the only WHO pre-qualified technology for a needle-free globally and that covers the WHO countries, which are something like 190 countries. Going back to needles and legislation, part of why we started as well is that there eventually were laws passed which require safety provisions for needles. There’s about a 65% risk for the patient and caregiver that as you’re finishing your injection and in between that moment and disposal, you may have a needlestick. That needlestick could contribute up to twenty bloodborne pathogens. Most commonly would be things like HIV and hepatitis.
Protecting the healthcare workers, protecting the patients from that exchange was key to why it was important to have safety measures. We’re fully safe. We have no needle. We don’t require necessarily specialized sharps disposal like needle-based delivery does. The laws that were passed in the United States eventually spread to the EU area and Brazil. Every country is a little bit different. When you go into a scenario, where there is no disposal, it’s a field setting or getting rid of hazardous waste ends up in the garbage dump, it’s incinerated and it goes into the air, we have a bit of an advantage there. We designed the syringe so that you can’t reuse it. There are no sharps, there is no metal to incinerate and then our injector is long life.
As a system, it’s efficient and beneficial and all of that economics help flow through to make sure that there are savings for every single injection, but for the user. In a Coronavirus scenario and we’re not talking about the United States. There are seven billion people on the planet with a highly variant virus that’s spreading. The objective is to have multiple vaccine solutions for this. If you can imagine, there are not even enough needles and glass packaging. There’s not enough anything. PharmaJet conserves a hugely important role in attracting needle-phobic patients, make it simple to give care. We’re particularly useful in mass immunization settings with the ability to process lots of patients. We capture 20% more typically out of the vials because of the engineering. We have great efficiencies that capture what waste would normally be in that needle cannula thing. This is a scenario where we all get to participate in finding a solution and we have some special features that make us relevant.
This is our second year offering Needle-Free flu shots, and we have had several people coming back requesting it again. Click To TweetAs you were commenting, 65% chance for the administrator of risk. All the people on the planet and the mechanics and logistics of getting some percentage of those people immunized. You have the administrator and if you’ve got 100 of them, the incidents of risk to each of those. I don’t know that it was as the risk to the caregiver as well understood as it is because you have a lot of the health caregivers that are at risk of the virus now.
Back to that statistic, in the US typically, a healthcare worker would need to report a needlestick, and a lot of times they don’t. It would be 1 in 7 healthcare workers in a given year would have a needlestick.
It makes you wonder what the real number is.
Much of the rest of the world, they might not be, but in certain literature in Africa, it’s been determined that up to 50% of the healthcare workers would be hepatitis positive. In places like South Africa, the burden of HIV is quite significant and 50% of the patients might be HIV positive. You start to see that this disease burden issue can be a real risk. If we can take out the issues associated with those hazards and then we can add to the efficiencies, we’ve seen teams of people working together, whether or not it’s the US, Pakistan, or Cambodia. When they work in teams, our technology tends to be about 2 to 3 times faster than needle-based delivery, so it’s faster patient processing. If we imagine a scenario where you might have a drive-by, instead of testing, it’s drive-by immunization. Roll your sleeve down, get your PharmaJet COVID shot. We’ve had that experience for influenza here. We don’t know yet about the vaccine cures that may come about, but we would very much like to be part of all of that and playing a role in multiple places and geographies.
I think of the mechanical advantage. In the military, I can remember lining up for processing for overseas movement and they would have all these stations and you basically lined all the soldiers up and they would tell you, “Roll your sleeves up, shut up, and get your shot.” They could process you a little faster, but still, it was a mechanically long process to get all that done. I think about that a lot. For you, you’re knee-deep in the vaccine landscape and you know the difference that exists in the standards of care. What do you see out there? What are your thoughts on that?
Universally, people go into healthcare because they want to help people and they want to make a difference. There are a few nurses I’ve observed that are a little bit like the grab and jab, efficiency, and get on with it. In general, people want a gentle experience or maybe the example you gave is military. Line up and shut up. I’ve observed more people standing in the needle-free line versus needle lines. In part, it’s for that reason. They’re also sometimes caregivers that positively choose that they want to provide needle-free injections versus needle-based delivery. While there might be multiple options, the venues are a place that probably wants to treat people with dignity, respect, but yet be efficient. The possibility thing for the United States, if you look at 2009 and H1N1, in most states, vaccines were not allowed to be given in the pharmacies.
Now all 50 states have approved for immunizations for pharmacies. That’s going to become a natural venue in addition to public health or other significant locations. If you look at some of the impoverished countries that are under-resourced, it will be field settings. Mass immunization could occur, neighborhoods to neighborhoods, door to door. We’ve had that experience in Pakistan where 500,000 children were immunized in five days by 1,100 caregiving teams. We’ve proven this efficiency and it’s probably safe to say that we’re confident that we could go into any environment, sophisticated or unsophisticated, and find that we could effectively immunize people and have a significant positive patient and healthcare experience.

Needle-Free Immunization: Disabled children tend not to have the opportunity to go to school and therefore tend not to have the opportunity for gainful employment.
I think about the concept we’re going to immunize 500,000 kids. You have this preconceived notion. You have your team set up and then you get the feedback from going through. Were there any a-ha revelations after doing that many kids with your teams?
What’s interesting is if you were to listen to my CEO Chris Cappello talk. By the way, he’s a little bit like a cofounder and he’s helped design our equipment. He’s an extraordinary engineer. He had the opportunity to train 50 master caregivers via Webex. They were in Karachi, Pakistan in the middle of our Colorado night and the connection kept breaking. His caregivers also had materials in front of them, the self-training materials that we’ve developed every time. Based on that two-hour period, those 50 master caregivers went off and trained 1,100 teams in one week. That following week, those teams immunized 500,000 kids in five days. That learning on the training side was invaluable. We designed it to be easy, ship it anywhere and somebody can take it out of the box, self-train with our little practice ball, 4 or 5 injections, twenty minutes, and then start immunizing.
Some of the other a-has are joyous because the healthcare teams are delighted that “the children didn’t cry” or if they knew, it didn’t matter. The injection process is that you have to be against the body before the trigger will be released and the energy creates that fluid stream. It’s safe. If you’re a parent, we’ve all experienced that when your child is in distress, it’s stressful for the parent. Consequently, there were numerous people that walked away saying, “Why didn’t we always do it like this?” They want every immunization to be this way. That’s a positive trend. You would want to keep bringing your child back for their immunization schedules if you knew that it was going to be a happy experience versus the other times when the kids go kicking and screaming. It’s no different than the dog going to the veterinarian. They know.
I was a Navy brat, and you’d go in for the Navy care. You’re going to go, “I’ve got to get my shots.” It was you kicking and screaming. There is no interest in going to repeat the performance. The message that must come from all of those children, there’s a generation, they’re going to talk to their children.
It’s like that Star Trek thing where if we’re old enough, we remember Star Trek and we go, “Great. Needle-free,” versus a younger person who might not know what that’s like. Their view is, “Why haven’t we always done it this way?” I’d like to think that we get to that point where it’s a little bit like the cell phone. If you never grew up with party lines or rotary phones, you have no idea about the party line.
Thinking about PharmaJet’s progress to where your business is now and in the technology, you’ve been doing this for a while and you’ve got a role. What role do you intend to play?
Science is a bit glacial sometimes. It does take tons of time to prove things. What we’re experiencing, by the way, with the caveat of Coronavirus vaccine solutions, it’s going to take time. We may have a solution that we think is pretty great or multiple solutions, but it does take time to follow the patients, understand protective immunity, make sure that if you need to boost your shot, that works. If the virus mutates, maybe it becomes like the annual flu mix that we might have Coronavirus vaccines annually going forward. Science again takes time. I would say that if you look at the last decade of our development where we’ve amassed many firsts and only it’s on a regulatory basis, scaled our device platforms, completed multiple clinical studies with existing vaccines, we’re entering into that era with our novel portfolio moving forward.
We all share the healthcare burden. Click To TweetWe have 67 human clinical studies underway, more than 50 collaboration partners. That’s large pharma, small pharma, academic, NGO, and government institutions like the NIH as an example. We’re up to foreign institutions as well. The roughly up to 100 novel vaccines and therapeutics moving forward, while that may take about a decade of time to see several of them reach commercial state. I envisioned that it will become a standard of care because in many cases there, those injectable medicines are not working well with needles. The job of a vaccine is to improve the antibody response and our fluid injection somehow does that well.
For several fold better than needle-based delivery, we’re finding that in nearly every case where these candidates reach the human clinical testing stage, needles are dropped altogether. We become the named and likely the only method of administration for those injectables. PharmaJet has a real role to play and will occupy a distinctive place in the future as these new treatments come to market. That’s my vision for the next decade on novel things. Wouldn’t it be great to look back a decade from now and say, “There isn’t any more incidence of polio?” To find that the basic healthcare in the world that includes measles, all kinds of infectious disease, that we’ve eradicated 1 or 2 of those diseases. WHO’s a priority is polio and then second would be measles.
I think about the landscape. I can remember talking to my great aunt about the Spanish flu and I talked to a guy out of Kansas not long ago, PhD type. He said the Spanish flu originated in Kansas. You go, “Why wasn’t it called the Kansas flu?” The experience of flu, we have a tendency to think that pandemics and flu strains are not that prevalent, maybe except for you. You’re in the field. We’ve got the flu. Going forward, I suspect we’ll have this transmission on a regular basis, for whatever reason. You look at it and if there was ever a wake-up call, we have one.
That is for sure. There’s been concern behind the scenes with governments for a long time and Mr. Bill Gates himself has made it clear that’s one of his biggest concerns. The concept of a pandemic, which means global, ends up being derived from a vicinity. If you look at influenza, a lot of the influenza strains start in Asia, particularly China. As time goes on during the course of a year, it morphs, moves, and changes because we’re all sharing that disease burden. We’re on different airplanes. It mutates. By the time it makes it to the United States, we have a flu mix that we think is about the right to protect us. If you look at the risk of Arctic Circle melting disease in the Tundra that we’ve never been exposed to in our lifetimes, no one has protective immunity against whatever that may be.
If you look at animals and the fact that in certain cases to see these viruses jump from animals into humans, in the Coronavirus family, SARS is thought to be associated with civets. MERS is thought to be associated with camels. COVID-19 is thought to be associated with bats. Coronaviruses, the common cold, but within there are several areas that historically weren’t something that human beings experience. This close proximity to animals, travel, and mosquitoes coming into places that have never been before. Zika would be a great example where we had a real scare that mosquitoes bringing Zika were coming into the United States and spreading the disease. By the way, they determined that’s sexually transmitted. It went in in one year through all 48 states with the exception of Alaska and Hawaii.
We’re going to see waves of concern and whether or not they reach the pandemic stage ends up being associated with surveillance in various countries. Trying to restrict travel like around the Ebola crisis. Sometimes certain things are carried in water supplies. It’s hard to transmit the water supply, but if it’s carried by humans and gets into another water supply. I don’t mean to be a doomsayer or I’m encouraged by the amount of collaboration around this pandemic. They think it’s going to change how science works and the ability to potentially fast track solutions that are incredible disease threats for our populations. It is important that that science continues to be well-funded and innovation is supported because it does take a long time and a lot of money to bring things to market.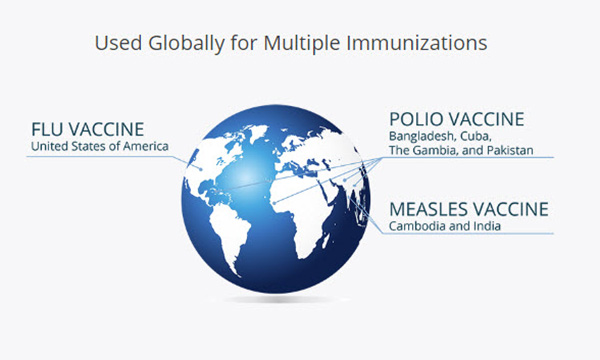
I was thinking as you were talking about herd immunity, which sounds like a bunch of cattle, but which may be a better analogy than we think. Let’s say that the vaccine is administered and PharmaJet’s doing their thing in vaccinating, herd immunity without vaccination and then they curve herd immunity with vaccination and the tipping point. I don’t know what percentage of the population would have to be vaccinated before it started to make a difference on the spread. I don’t want it around out there and I’m vaccinated. I’m not spreading it to any quantity of people. Have you seen any work on that where people are trying to model what that looks like?
I have and it’s important to point out that in certain cases if you don’t have it and you don’t share tissue fluids, you can’t get it. Hepatitis or HIV would be an example of that. There are many things that are respiratory illnesses that are spread like measles, tuberculosis, influenza, our Coronavirus crisis. Let’s talk about influenza. It tends to be that 65% of the population is healthy and immunized. The rest of the population is generally healthy. There are certain diseases, viruses, or respiratory illnesses that have a higher spread rate where therefore the protective immunity level relates to how many people are immunized. In the case of measles, it’s typically about 90%. In the case of polio, it’s 95%. We don’t yet know what it will be in Coronavirus. Given how quickly this has spread and mutated, the chances are high that we’re going to need to see very widespread immunization for a good long time to make sure that the disease is arrested. I don’t know that it can ever be eradicated and that’s the difficult part.
We’ve not been able to get rid of the “flu.” One year’s flu vaccine is the blue one. The next year is the green one. Did it work? Not perfectly, but it was better than not. I suspect in the days when we didn’t have travel as we have now, cruise ships, airlines, it would take like the Spanish flu basically got to Europe with World War I, as I understand it. Had we not had all the troops shipped and all that, it might not have been as big a deal as it was.
That was then and this is now. We have such tremendous commerce and are connected that it does allow for the disease to be borderless.
It’s democratic. It doesn’t matter who you are. For PharmaJet, you have been knee-deep in global polio. Where do you see you guys on that scale? Are you getting close to getting polio done in the world? What’s the biggest barrier to you getting that done?
Universally, people go into healthcare because they really want to help people. Click To TweetThe oral drops have been able to bring the disease incidents down to a handful, a few hundred cases per year that have been reported, which is extraordinary. However, the poliovirus lives in every sewage and water supply in Pakistan, as an example, in an endemic country. It requires a lot of coordinated immunization for a long time, along with probably infrastructure investments in sewage treatment and things. Yet there is vaccine-derived polio. Despite that these oral drops are helping to bring the disease incidents down, every once in a while, an individual immunized manifests polio. You have to move to the inactivated vaccine to eradicate that disease fully. The thinking by the World Health Organization is after the last polio incidents example has been observed, for at least a couple of years, they only then will completely destroy the stockpile of oral drops and move to the inactivated vaccine. We’ll need to continue to immunize for at least a decade or two before they will declare that polio is eradicated.
It’s a generational project.
It is generational, maybe in the water supplies. It’s not just polio, but there’s a family called Enteroviruses. These viruses live in the human gut, probably lives in the human blood and therefore it gets into the water and sewage. In certain water supplies, there are specific Enteroviruses which do cause paralysis. They’re specific to those water supplies. It’s a whole group like the Coronavirus family. There are Enterovirus vaccine candidates under development in different parts of the world. Polio is horrifying and it was in most of the world half a century ago and vastly reduced now, but that last mile and eradication are important. Smallpox is the only other disease that’s been eradicated from the planet so far, and polio will be the second.
Wasn’t it down in Georgia that Roosevelt went to “treat or deal” with his symptoms? Wasn’t that where he went? That’s what I remember as a kid and I can remember going through the process. I can remember my parents were excited about it. We were talking about the significance of the reduced dosage use when you are administering a vaccine. What do you think that means? What does that mean to PharmaJet?
It gives us a huge competitive advantage because to inject into the intradermal layer of tissue, which is about 1.5 to 3 millimeters of space, with a needle is hard and it’s painful for the patient. We’ve designed our technology that it’s a simple push and click basically up against the body. You release the trigger and it’s done faster than your nervous system can register a response. It’s comfortable. We don’t take the sting out of whatever’s being injected, but it’s a huge competitive advantage versus needle-based delivery. People can’t deliver the needle-based delivery, but in part, we would all like to have a more pleasant experience and faster patient processing. We’ve had time trials and evaluations in places like Gambia and Pakistan where individuals working, not teams, tended to be 3 to 4 times faster than needle-based delivery.
We won’t fully eradicate the use of needles, but we certainly have a huge competitive advantage. Not to exclude the economics around that. If we’re able to reduce the dose by moving from the muscle to the skin, in our case for polio, 60% less is superior to full dose. We also then functionally get 20% more out of the vials because we’ve engineered out the waste of what type you would experience with needles. That plows back a positive return for every immunization. There have been health economists that have documented their view of the savings that we create, which is about 30% for every single PharmaJet needle-free injection for polio. A full dose in the muscle versus PharmaJet’s injections into the skin, that 30% savings end up paying for the cost of the equipment. It creates a sustainable model for these countries to adopt, to afford eradication essentially.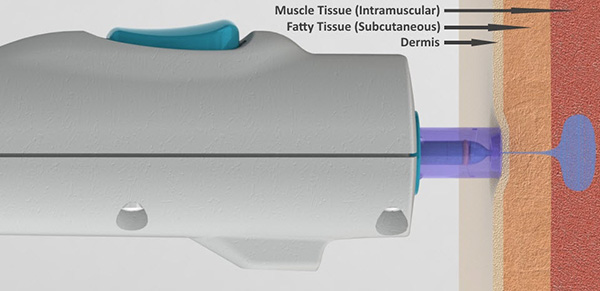
I’m thinking, “It’s faster. It works better. Culturally, it’s acceptable.” What’s the pushback? For me, I’m here going along, “Why isn’t everybody doing this?”
First, I guess because the polio vaccine would be in multivalent vaccines that we use as a standard of care here. It’s not a single vaccine. We’re not using intradermal polio vaccines in the United States. It’s much of the developing world. In fact, there’s a World Health Association vote that all 151 countries agreed of them that they would migrate from the oral drops to the injectable vaccine, but the economy has taken a toll on how quickly this has come to market. It’s a big financial hurdle for many of these countries. There hasn’t been enough injectable inactivated vaccine supply. This creative development around this plan to eradicate the disease is kicking off commercially now. That’s why I say sometimes science is glacial.
It takes a long time to prove clinical studies. It took us at least two years to scale our technology and complete our audits before we could start producing our product. Now we’re engaged with multiple countries. Many of them are GAVI member countries. GAVI stands for Global Alliance Vaccine Initiative. It’s funded by the Gates Foundation and the fifteen wealthiest countries in the world. They support these immunization costs with these impoverished countries that need financial help to adopt something like the standard of care. The deal is that those countries agree upfront that if they have that subsidization after several years of immunization, they’re on their own. We’re engaged therewith inactivated polio vaccine in a fractional dose using our device with more than twenty countries that are engaged in these GAVI applications to make it a standard of care in their country.
Bob, if you give me the opportunity to tell you all about it, I’d say that we’ll be in multiple additional countries and those we’ve already experienced. I’m excited about the example in Pakistan because the first opportunity was a little field assessment. The next opportunity was 500,000 children immunized in five days. We shipped the product because there was a plan to immunize 1.5 million kids in a week. It will start to mushroom and grow and it will be a joy to share what the outcome of all of that is. Also, it’s not big country. We’ve had experiences in places like Cuba, a high standard healthcare system with tremendous nurses.
We were involved so far in 33 clinics, immunizing all day, every day their patients coming through for standard routine immunizations. Now, Cuba’s moving forward to adopt it as a standard of care for the country, which is exciting. Both cases, small countries, large countries. We don’t care much about the venue. We want to make a contribution to health, wellbeing, safety, and savings. PharmaJet is a for-profit business, so don’t get me wrong. We need more investment in order to continue to feed our development capacity. The fact that it’s a win-win for everyone makes us essentially a sustainable business model. We can do well, we can do good, and we can create returns for our investors.
I think about the economic benefit. If you’re a caregiver for an Alzheimer’s patient, your life is dramatically and forever changed, and so on. If you’re a caregiver for somebody with COVID virus, your life is different and changed and they’re segregated in your house and you have to behave differently. With polio, I can imagine it’s a lifelong sentence. The person with polio is impoverished unless they’re incredibly fortunate. I think about that economic improvement or value.
There’s a high correlation, sadly, where disabled children tend not to have the opportunity to go to school and therefore tend not to have the opportunity for gainful employment. If you can imagine what your life would be like if your child could not walk, it would be devastating. There are statistics in all kinds of categories. It’s the same with autism. If your child is highly autistic, it destroys the family fabric because it’s stressful but particularly important is the need to be functional, which allows people to be educated and to work. That is universal regardless of degree and circumstance.
Ignorance is incredibly expensive, which is a fair understatement, I’d say. In looking at PharmaJet and with the pandemic, how do you see you guys fitting in with these pandemic issue challenges?
It’s something that we’ve been working on quietly and I don’t want to over-promise that we’re going to have the solution, but we’re part of fourteen separate pharmaceutical developments for Coronavirus. We had a check-in with BARDA, who was in charge of pandemic preparedness. We were already working on pandemic preparedness for influenza with them and the FDA and that quickly turned to Coronavirus. There are multiple innovations going on, some reported 100 candidates in the world, but we have several partners that are working in different approaches to vaccine development. We have multiple partners in different geographies. The US, several in Europe, Middle East, Asia, and it’s potentially an opportunity where anything that gets to the stage of proof of concept.
We could include PharmaJet as an alternative method of administration in that clinical study to demonstrate that needle and needle-free are the same so that we can be part of the solution. Let alone potentially being able to reduce the dose. Many of our novel vaccine development partners find out that the immune response tends to be similar to both of our devices. A 0.5 milliliters injected into the intramuscular space is similar to 0.1 milliliters into your skin. Functionally, if we could stretch the dose by 80% and get the same immune response and if we can also utilize the fact that we eliminate waste and get an extra couple of doses out of that vial and plow back that positive ROI or immunize more people. There’s a lot of development coming that we’re excited about because we intend to be part of the solution.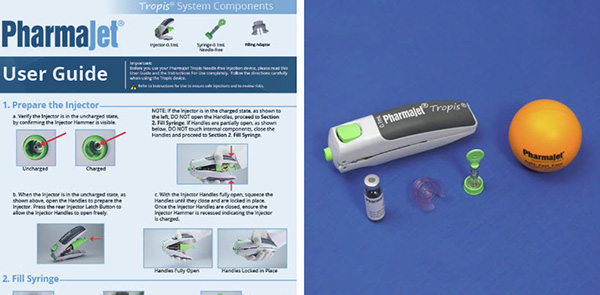
The mechanics take less, go in faster, don’t have to have a highly skilled administrator. The risk of administration is lower. When you think about the compound effect of all of that, if you get 5% here better, 2% here better, 3% faster here, and all of a sudden you start looking and multiply that by millions of individuals. It gets incredibly compelling.
We can save a lot of money and we can immunize more people. That is true. When my mother started, she related how in healthcare it always has to be cheaper. You’re always looking for innovations that save you money. As much as we’re not relatively expensive, it’s not dissimilar to a needle, at least in terms of US pricing, we’ve been able to effectively compete against $0.05 needles in the rest of the world and still save 30% on immunizations. The cost of the vaccine is a much different scenario. Huge manufacturing scale-up costs. If we could stretch the dose either, they have to manufacture less of it or they can’t immunize more people. There’s always this win-win opportunity in our view. I want to touch on the fact that, why has it taken so long? The truth is that I don’t think that the vaccine manufacturer loves us when we tell them that we can get more doses out of their vials or reduce the dose.
It’s like in the case of polio, we are not on the vaccine labels for the vaccine companies, but the WHO cares a lot about the cost of that eradication. In this circumstance, we will find that because we facilitate vaccines coming to the market, we facilitate more people showing up and participating in reaching that herd immunity level and then stretching the dose, whether or not it’s more vaccine out of the vial or intradermal versus intramuscular, that will set the mark of being able to prove that this needle-free capability. It’s important to the true cost of healthcare. We can play a role, and we’re not going to eliminate needles, but we can play an important role.
The psychology of any family like, “I got my vaccination.” “What would it feel like?” “What do you mean?”
Some people walk away and they say, “I didn’t feel that.” In some cases, it’s a little bit like a rubber band snap, but it’s comfortable.
As you’re going forward and you’ve been working on polio and the pandemic, what type of support are you getting? What do you need that might be getting in the way of getting towards your goals?
Funding is super important and in the medical technology world, life science world, traditionally you’d find that companies are not profitable for a number of years because they’re still adding layers of development that require funding and time. The truth is we have needle-free manufacturing capabilities, but it needs to be larger and therefore we need third-party funding in order to grow our capacity. We contract manufacture. It’s not that we need to build more plants. We have robotics and molds in it. On a relative basis, our next scale-up plan is to add a 45 million syringe throughput.
It’s about $4 million investments. Rule of thumb, if you have a ten million syringe monthly output, 120 million syringes per year, and an additional 50,000 injectors, it might be $20 million. Compared to what might need to be invested in the vaccine manufacturing capacity, if you crunch the numbers, I’m going to guess that the return on our investment is extraordinary. Not to mention that for our shareholders, we intend to be playing a role. We intend to be a building block as a company for a larger company to own PharmaJet eventually. The ROI for the investment is stunning. That’s it. It’s a great return.
I think about the expense of the economy worldwide and this is not the first one. It’s not going to be the last one. It’s going to be an ongoing issue. I suspect that the wisdom of the crowd working all on vaccine development, I suspect there’s going to be some a-has that come out of this that will likely speed up the development of vaccines. At least I’d like to think so.
I’d like to think so too. One thing I should call out is that we’ve been supported by high net worth and family office investors to date. I come from a private equity background historically prior to PharmaJet. When the world crashes, unfortunately, certain funding mechanisms dry up. We replace them. In the case of institutional investors, many of them are worried about their existing portfolio and the impact of this Coronavirus scenario on those companies and their survival. We continue to be supported with high net worth and family office investors. We certainly have an institutional interest, but it’s critical that people understand that there’s a lot of empathy with what we do and why we do it.
We’re oriented to be a sustainable and profitable business eventually. There will be more groups multilaterally coming in to fill some of those funding gaps because it’s enormously important to support the health systems and make sure that the infrastructure doesn’t fall apart because of a lack of investments. We need our healthcare workers. We need venues. That’s not in the United States but in the rest of the world. I’m confident that innovation, not just PharmaJet, in this scenario will continue to be funded. The government funding is probably some of the more important funding because it’s a much larger initiative that’s being coordinated among multiple jurisdictions, technologies, and agencies like the FDA.
Besides clean water, immunization is the cheapest form of preventable health. Click To TweetI’ve been harassing you off and on for a couple of years. You’ve been busy doing what you do. I’m honored that you came. I’m appreciative and I’m excited about what you’re doing. To wrap this up, what do you think the future of immunizations is going to look like 3, 5, 10 years down the road?
It’s funny because I don’t think you harassed me too much, but I kept saying, “Not yet, but I have things to tell you. It’s going to happen and we’ll have the opportunity.” Immunization will become more mainstream in some of these untraditional venues. Going back to the fact that in 2009 with H1N1 here, we didn’t have immunization in these pharmacy chains that are on every street corner. There are those developments in multiple countries that we probably will see become important venues. I also think that there is some creative thinking along the lines of how do you make it important and expedient for the patients. Rapid immunization versus routine immunization. I do hope that people’s awareness around immunization is that it is standard of care. Besides clean water, it’s the cheapest form of preventable health. Instant immunization is probably key to US, Europe, and some of the more developed economies. Being able to make sure that it’s standard of care, routine immunization, and that PharmaJet’s part of that so that we inspire immunization, keep people safe is what is going to happen.
Heather, I hope so. I’m appreciative of you taking the time to come and tell us your story. I look forward to doing this again. As you get down the road and more things come to pass and there are some updates, we’ll take and do this again, but I wish you much success. Thank you for taking the time to come and be a guest. Before I forget, how do people find you on social media?
LinkedIn for sure. We have a PharmaJet LinkedIn page and you can probably look up Heather Callender-Potters and find my profile. We have a robust website with lots of training materials and then contact information for whoever you want to talk to whether or not it’s our clinical team or our sales team. Those are the two easiest avenues. We have a host of YouTube videos to show you what patient experience is like, as well as training and use of the device. I hope people will have an opportunity to either reach out or learn more about us in that way.
Thank you for taking the time. I appreciate it.
Important Links:
- Bill & Melinda Gates Foundation
- CDC
- GAVI
- BARDA
- PharmaJet – LinkedIn
- Heather Callender-Potters – LinkedIn
- YouTube – PharmaJet
- https://YouTu.be/5VSUdcsh0OE – 60 10406 002A Tropis Educational Video
- https://PharmaJet.com/
About Heather Callender-Potters

Ms. Callender-Potters has a Bachelor of Arts degree in International Management from Claremont McKenna College and an MBA from Wharton, the University of Pennsylvania. One of the co-founders of the company, Heather has over 25 years of active investment experience including Private Equity fund management and international investment (BCEE; Enterprise Investors) across multiple jurisdictions and has managed individual investments and financial investor consortiums, ranging from $1 million to an excess of $100 million. She has also held board positions with several companies acro
ss a variety of industries ranging from auto-parts to systems integration, publishing, and light-manufacturing.
Love the show? Subscribe, rate, review, and share!
Join the Business Leaders Podcast Community today: